In the
exhaustive list of complications of long term steroids, we find a disabling
condition called Avascular necrosis (AVN) of the femur head. In Ophthalmology,
steroids are inevitable in many diseases, which include Scleritis, posterior
uveitis, uveal effusion syndrome, Eale’s disease, optic neuritis, exudative
retinal detachment and inflammatory orbital disease etc. We present a case of
avascular necrosis of femur head in an 18-year old medical student who
presented with Eale’s disease. Eale’s disease is common in Asian sub-continent
and steroids with anti tubercular therapy are the mainstay of treatment. In
uniocular Eale’s disease involving a single quadrant of retina, it is preferable
to use periocular and intravitreal steroids but when it comes to recurrent and
four quadrant disease (as seen in this particular case), oral steroids have to
be given.
Other causes of avascular necrosis with possible pathogenesis are discussed
and recommendations are made for early detection of AVN.
CASE REPORT
An 18-year old Pakistani
female came to eye outpatient department with history of floaters in her right
eye for a week. On examination, her visual acuity was 6/6 partial in right eye
and 6/6 in her left eye. IOP were 14 mm of mercury in each eye. Anterior
segment was normal. On fundoscopy, there was inferior hemiretinal branch vein
occlusion in right eye figure 1 and 2. Left eye was normal. Patient was
investigated for hematological and autoimmune abnormalities. Complete blood
with ESR, urine, stool, chest X-ray, RA factor, ANA, cANCA, pANCA, protein C,
protein S and anti thrombin III were normal. Patient was diagnosed as Eale’s
disease and oral prednisolone, 1 mg/kg body weight was started as a short
course. After three months patient came with recent onset of floaters in the
right eye. Visual acuity was 6/24 and fundus examination revealed central retinal
vein occlusion. There were white cells in vitreous and severe perivasculitis
was also seen. OCT showed frank macular edema, figure 3. Left eye was normal. Intravitreal
Bevacizumab was given and oral steroids were started again to control
vasculitis. Patient was prescribed ATT for nine months. After three months, vision improved to 6/6
partial in the right eye. Fundoscopy revealed resolution of retinal hemorrhages
and macular edema was settled. A neovascular frond was visible at supero-nasal
quadrant of retina. Pan retinal photocoagulation was done and oral steroids
were gradually tapered. After three months, she complained of pain in the hip
joint, which was not settled with any pain killer. She consulted an orthopedic
surgeon who diagnosed Avascular necrosis (AVN) of both hip joints. Oral
steroids were stopped and she underwent core decompression of both hip joints
with external implant in the right hip. At
her first follow up visit, the right hip joint had a progressive AVN and the disease
in left hip joint was stable. After one year, she again developed sudden loss
of vision in the right eye. Examination revealed dense intra gel and sub
hyaloid hemorrhage. On B-scan retina was intact. The patient needed anti-VEGF
in her eye to combat abnormal vascularization, which was the cause of vitreous
hemorrhage. Systemic absorption of anti-VEGF could have a deleterious effect on
the hip joint, which required Vascular endothelial growth factor to prevent
further progression of AVN. We gave intravitreal ranibizumab because of its lesser
systemic absorption than bevacizumab. After one month the hemorrhage had resolved
and visual acuity was restored to 6/9 partial. Argon laser was augmented.
The patient is ophthalmologically stable at the time of this
report and regular follow up by the orthopedic surgeon is still going on.
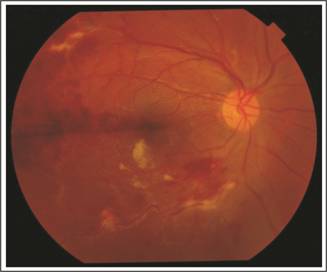
Fig.
1: Right eye showing branch retinal vein occlusion with peri-vascular
sheathing.
DISCUSSION
Avascular
necrosis (AVN) of femoral head was first described by Alexander Munro in 1738.
In 1835, Cruveilhier described the interruption of blood flow as the cause of
AVN. With advancement in diagnostic techniques, number of AVN cases has
considerably increased.
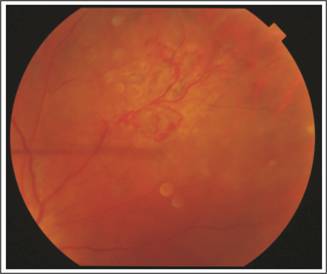
Fig.
2: Peripheral neovascular frond, which was present at 2 O’clock
position of the right eye. Laser marks are also seen in the figure.
The two most
important factors which contribute to AVN are corticosteroids and alcohol
intake1,2. While corticosteroids induced AVN mainly affects the
femoral head, the cause is not yet confirmed. It is hypothesized that fat cell
hypertrophy and fat embolism can result in blood compromise to the femoral
head.
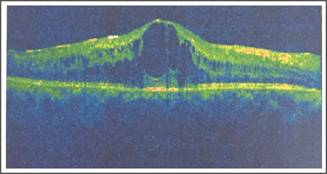
Fig.
3: OCT of the right eye showing cystoid macular edema, which
developed after BRVO.
Steroids are the
sole treatment in several of the medical conditions. Literature shows that the
commonest conditions in which steroid induced AVN is seen, are post renal
transplant and SLE3. In ophthalmology, steroids are used in ocular
manifestations of many collagen vascular diseases for example; peripheral
ulcerative keratitis, uveitis, Scleritis and epi-scleritis. Exudative retinal
detachments, retino-choroiditis, optic neuritis and Eale’s disease are some of
the other ocular conditions in which systemic steroids are the mainstay of
treatment. None of the above-mentioned disease is reported in literature for
steroid induced AVN.
Although high daily doses3,
cumulative dose4 and long duration of steroid administration are the
main contributing factors, there is no consensus on the safe dose and minimum
safe duration of steroid use. However, AVN does not occur in majority of cases.
It can be because of other contributing factors like hyperuricemia in psoriasis and hyperlipidemias in SLE. A study was
carried out in China, which showed a positive relation between atherosclerosis,
male gender, urban residence, family history of osteonecrosis of the femoral
head, heavy smoking, alcohol abuse, glucorticoid intake, overweight and
osteonecrosis of femoral head5. Vascular compromise could also be from
a clotting disorder or genetic abnormality6.
In this particular
patient, underlying vasculitis (which was seen in
the eye as Eale’s disease) could have been the contributing factor for AVN.
Vasculitis can cause hyper coagulable state with resulting sludging of blood
vessels and embolization. Steroids are also responsible for hyperlipidemia,
which can also contribute to bone infarction. Role of lipid lowering agents in
the animal models gives some clue about the high lipids levels as a
contributing factor in AVN7.
Studies have shown that vascular
endothelial growth factor, which is meant for bone repair and angiogenesis, is
decreased by up to 45% with the use of steroids8. The dilemma in our
patient was that she started to develop new vessels in the eye, which caused
vitreous hemorrhage. We had to give her Anti-VEGF injection in the vitreous
cavity. There is considerable absorption of Anti-VEGF agents in the systemic
circulation after intra vitreal injection. This could adversely affect the
already compromised vascular supply of the hip joint, which needed vascular
support. Hence, intravitreal ranibizumab was given which has lesser systemic
absorption.
This patient used oral steroids off and on for six months because
of her recurrent central retinal vein occlusions. However, AVN with daily doses
as low as 5mg prednisolone and duration as short as 7 days is also described in
literature9. Such reports favor the idea that the underlying disease
for which the steroids are given can be the contributing factor in AVN.
CONCLUSION
Rare complication is not rare for the
person who develops it. Surgeons and physicians should be vigilant in
prescribing any medicine having, although rare but, serious complications. MRI
should be recommended after six months of steroid intake (irrespective of the
dose of steroid used).
There are certain situations where you need the effect of a drug
at one part of the body and want to avoid the drug effects at other part. In
such medical dilemmas, risk benefit ratio should be carefully calculated.
Author’s
Affiliation
Dr. Tayyaba Gul Malik
FCPS, Professor
Ophthalmology,
RLMC
Dr. Muhammad Khalil
FCPS, Associate Professor
Ophthalmogy, LMDC
Role of Authors
Dr. Tayyaba Gul Malik
Data acquisition, manuscript writing, final review
Dr. Muhammad Khalil
Data acquisition, manuscript writing
REFERENCES
1.
Sonoda K, Yamamoto T, Motomura G, Hamai
S, Karasuyama K, Kubo Y, Iwamoto Y. Bilateral corticosteroid-induced
osteonecrosis of the femoral head detected at a 6-week interval. Springerplus. 2015; 4: 662.
2.
Flouzat CH, Roubineau F, Heyberger C, Bouthors
C, Hernigou P. Multifocal osteonecrosis related to corticosteroid: ten years
later, risk of progression and observation of subsequent new osteonecroses. Int
Orthop. 2016; 40 (4): 669-72.
3.
Drescher W, Schlieper G, Floege J, Eitner
F. Steroid-related
osteonecrosis – an update. Nephrol Dial
Transplant. 2011; 26 (9): 2728–31.
4.
Sayarlioglu M, Yuzbasioglu N, Inanc M, Kamali S, Cefle A, Karaman O, Onat AM, Avan R, Cetin GY, Gul A, Ocal L, Aral O. Risk factors for avascular bone necrosis in
patients with systemic lupus erythematosus. Rheumatol Int. 2012; 32 (1): 177–82.
5.
Zhao DW, Yu M, Hu K, Wang W, Yang L, Wang BJ, Gao XH, Guo YM, Xu YQ, Wei YS, Tian SM, Yang F, Wang N, Huang SB, Xie H, Wei XW, Jiang HS, Zang YQ, Ai J, Chen YL, Lei GH, Li YJ, Tian G, Li ZS, Cao Y, Ma L. Prevalence of Nontraumatic Osteonecrosis of the Femoral Head
and its Associated Risk Factors in the Chinese Population: Results from a
Nationally Representative Survey. Chinese Medical Journal, 2015; 128 (21):
2843-50.
6.
Zhao D, Cui D, Wang B, et al. Treatment of early stage osteonecrosis of the
femoral head with autologous implantation of bone marrow-derived and cultured mesenchymal
stem cells. Bone, 2012; 50: 325–330.
7.
Iwakiri K, Oda Y, Kaneshiro Y, et al. Effect of simvastatin on steroid inudced
osteonecrosis evidenced by the seum lipid level and hepatic cytochrome P4503A
in a rabbit model. J Orthop Sci. 2008; 13 (5): 463–8.
8.
Kerachian MA, Séguin C, Harvey EJ. Glucocorticoids in osteonecrosis of
the femoral head: a new understanding of the mechanisms of action. J Steroid
Biochem and Mol Bio. 2009; 114: 121-28.
9.
Anderton, J.M. and Helm, R. Multiple joint osteonecrosia following
short-term steroid therapy; case report- J. Bone Joint Surg. 1982; 64-A: 39.